Does an X-ray show a bulging disc?

What is a Herniated Disk?
A herniated disk occurs when the ‘cushions’ (intervertebral disks) between the bones of the spine (vertebrae) weaken or tear. This causes the inside of the ‘cushion’ to budge (herniate) out of normal position. When the bulge occurs, this may cause a range of nerve-related signs and symptoms if surrounding nerves are compressed. These ‘cushions’ are soft tissue sitting between bones.
Risk Factors of Development
- Aging: herniated disks are most common in people aged 35 to 55
- Genetics: individuals may have a family history of early onset herniated disks, or many family members with a history of a herniated disk.
Lifestyle: heavy lifting, or excessive bending or twisting of the spine (work, sports)
Signs and Symptoms
- Back pain
- Numbness or tingling (arms, fingers, legs)
- Frequent urination
- Bowel or bladder incontinence
- Headache
- Severe leg pain or sciatica (lumbar disk herniation)
Diagnosis
A throughout medical history and physical exam are important for a health care provider to determine any imaging needed for diagnosis. The most common imaging modality is an MRI (magnetic resonance imaging), as it will show the medical provider the condition of the soft tissue of the spine and neck.
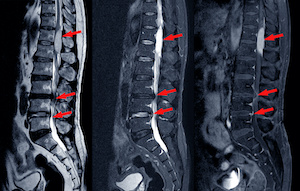
An X-Ray CANNOT be used to diagnose a bulging or herniated disk
X-Rays are most commonly used to assess the condition of bones and joints. An X-Ray may be ordered for the diagnosis of a tumor, arthritis, or fracture. Unlike an MRI, an X-Ray is not sensitive to assess the condition of the soft tissue.
Conservative treatment is most common
May include bedrest (for less than 1-2 days), heating pads, medication (NSAIDs or muscle relaxants), physical therapy, and aerobic exercises (after 1-2 weeks). If conservative treatments do not relieve symptoms, a your provider may recommend epidural steroid injections.
Surgical Interventions
- Indication:
- Loss of bowel or bladder control
- Progressive nerve damage
- Unrelenting pain after conservative measures
- Most common surgical treatment: remove the intervertebral disk (diskectomy)
- Less invasive surgical treatment: disk removal with an incision and hollow tube insertion to remove the intervertebral disk.
Summary
- Occurs when intervertebral disks between spine bones weaken, causing a bulge that can compress nearby nerves.
- Most common in people aged 35 to 55.
- Genetics may play a role, with a family history of early-onset herniated disks.
- Back pain, numbness, or tingling in arms, fingers, or legs.
- Frequent urination, bowel or bladder incontinence.
- Medical history and physical exam are crucial.
- MRI is the most common imaging modality to assess soft tissue condition.
- X-rays cannot diagnose a bulging or herniated disk; they are suitable for bone and joint conditions.
- Includes bedrest (for less than 1-2 days), heating pads, medication (NSAIDs or muscle relaxants), physical therapy, and aerobic exercises (after 1-2 weeks).
- If symptoms persist, epidural steroid injections may be recommended.
- Indications include loss of bowel or bladder control, progressive nerve damage, or unrelenting pain after conservative measures.
Take the first step towards strengthen your health by scheduling an appointment with our medical provider through Umedoc today.
This article reviewed by Dr. Jim Liu, MD and Ms. Deb Dooley, APRN.
There’s nothing more important than our good health – that’s our principal capital asset.
#medical #telehealth #umedoc






