Food Allergy vs. Food Intolerance: A Comprehensive Guide to Understanding Your Body’s Reactions
When your body reacts negatively to a certain food, it can be confusing and alarming. Is it a food allergy, or is it a food intolerance? The symptoms can sometimes overlap, but the distinction between these two conditions is critical. A food allergy is an immune system response that can be severe or even life-threatening, while a food intolerance is a digestive issue that is generally less serious. Understanding the difference is the first step toward a proper diagnosis and effective management.
This guide (updated for 2025) will break down the key differences between a food allergy and a food intolerance, help you recognize the signs of each, and outline the steps to take for an accurate diagnosis.
Understanding the Core Difference: The Immune System
The fundamental difference between a food allergy and a food intolerance lies in the body’s reaction system:
Symptoms: Are generally confined to the digestive system, including gas, bloating, abdominal pain, and diarrhea.
Food Allergy (Immune System Reaction): This is an immune-mediated response. When you eat a trigger food, your immune system mistakenly identifies the food’s protein as a harmful invader. It produces antibodies (most commonly IgE antibodies) to fight it. The next time you eat that food, the IgE antibodies release chemicals like histamine, which cause a cascade of symptoms.
Onset: Symptoms are often immediate, appearing within minutes to a couple of hours after eating.
Amount: Even a tiny amount of the food can trigger a severe reaction.
Symptoms: Involve multiple body systems, including the skin (hives, swelling), respiratory system (wheezing, difficulty breathing), and gastrointestinal tract (vomiting). The most severe reaction is anaphylaxis, a life-threatening, whole-body allergic response.
Food Intolerance (Digestive System Reaction): This is a digestive issue, not an immune response. It occurs when your body lacks the proper enzymes to break down a certain food, or when a food’s natural chemical causes a negative reaction. A classic example is lactose intolerance, where the body doesn’t produce enough of the enzyme lactase to digest milk sugar.
Onset: Symptoms are typically delayed, appearing several hours after eating.
Amount: The severity of symptoms is often dose-dependent. A small amount of the food may be tolerated, while a larger amount will cause a reaction.
Learn more about food allergies from our comprehensive PDF document.

Common Culprits and Diagnostic Pathways
Common Food Allergens: While any food can be an allergen, the “Big Nine” account for most allergic reactions in the United States: milk, eggs, peanuts, tree nuts, wheat, soy, sesame, fish, and shellfish.
Common Food Intolerances:
- Lactose: Found in dairy products.
- Gluten: The protein found in wheat, barley, and rye. Celiac disease is an autoimmune condition triggered by gluten, but a non-celiac gluten sensitivity is a form of intolerance.
- FODMAPs: A group of carbohydrates found in various foods, including certain fruits, vegetables, and grains.
- Sulfites: A preservative found in dried fruits, wine, and some processed foods.
How to Get an Accurate Diagnosis:
- For Food Allergies: A detailed patient history is the first step. An allergist may perform a skin prick test or a blood test to check for IgE antibodies. In some cases, a medically supervised oral food challenge is performed to confirm the allergy.
- For Food Intolerances: There are no reliable skin or blood tests for most intolerances. Diagnosis typically involves an elimination diet, where the suspected food is removed and then slowly reintroduced to see if symptoms return.
Management and Long-Term Implications
- Managing Allergies: Once diagnosed, strict avoidance of the allergen is essential. For individuals with a severe allergy, carrying an epinephrine auto-injector (like an EpiPen) is a life-saving measure.
- Managing Intolerances: Management often involves limiting the trigger food or taking supplements (like lactase tablets) to help with digestion.
A 2025 consensus statement from the American College of Allergy, Asthma & Immunology (ACAAI) highlights the importance of professional diagnosis to avoid unnecessary food restrictions, which can lead to nutritional deficiencies.
Conclusions and Key Takeaways
- A food allergy is a potentially life-threatening immune system reaction, while a food intolerance is a digestive issue.
- Allergy symptoms are often immediate and affect multiple body systems; intolerance symptoms are delayed and primarily affect the gut.
- Diagnosis for allergies is done through skin or blood tests, while intolerances are usually identified with elimination diets.
- Strict avoidance is necessary for allergies, while intolerances can often be managed by reducing intake of the trigger food.
Trusted References
- American College of Allergy, Asthma & Immunology (ACAAI). acaai.org
- Food Allergy Research & Education (FARE). www.foodallergy.org
- Mayo Clinic. www.mayoclinic.org (Search for “food allergy” and “food intolerance.”)
- Journal of Allergy and Clinical Immunology. (For current research on food allergies.)
Learn more about food allergies from our comprehensive PDF document.
About Umedoc Health Blog
At Umedoc, we’re committed to providing updated, accurate, and accessible health information to empower your wellness decisions. For more tips, health updates, and medical guidance, subscribe or bookmark our blog today.
This article reviewed by Dr. Jim Liu, MD.
There’s nothing more important than our good health – that’s our principal capital asset.
#medical #telehealth #umedoc #ecnoglutide #GLP #weight loss #Wegovy #diet

Recent Post
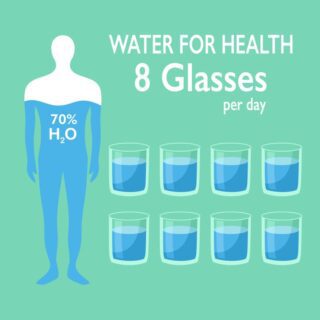
- The Liquid Advantage: Hydration, Thermogenesis, and Appetite Control
- The Hormonal Clock: Why Sleep is the Secret Ingredient to Fat Loss
- The Metabolic Shield: Preserving Muscle to Prevent Weight-Loss Rebound
- The Flamingo Test: Why You Should Stand on One Leg
- The “Natural Ozempic”: Why Fiber is the Hunger Crusher