Demystifying Eczema: A Guide to Managing Itchy, Inflamed Skin

Eczema, also known as atopic dermatitis, is a chronic skin condition characterized by dry, itchy, and inflamed patches of skin. While it can affect anyone, the warm, humid climate of Fort Myers, Florida, can present unique challenges for those managing eczema, as heat and sweat can sometimes trigger flare-ups. Understanding the nuances of eczema, its triggers, and effective management strategies is key to finding relief and improving quality of life.
This guide (updated for 2025) clearly outlines what you need to know about recognizing eczema symptoms, common triggers in our climate, and comprehensive strategies for managing this persistent skin condition.
Understanding Eczema (Atopic Dermatitis)
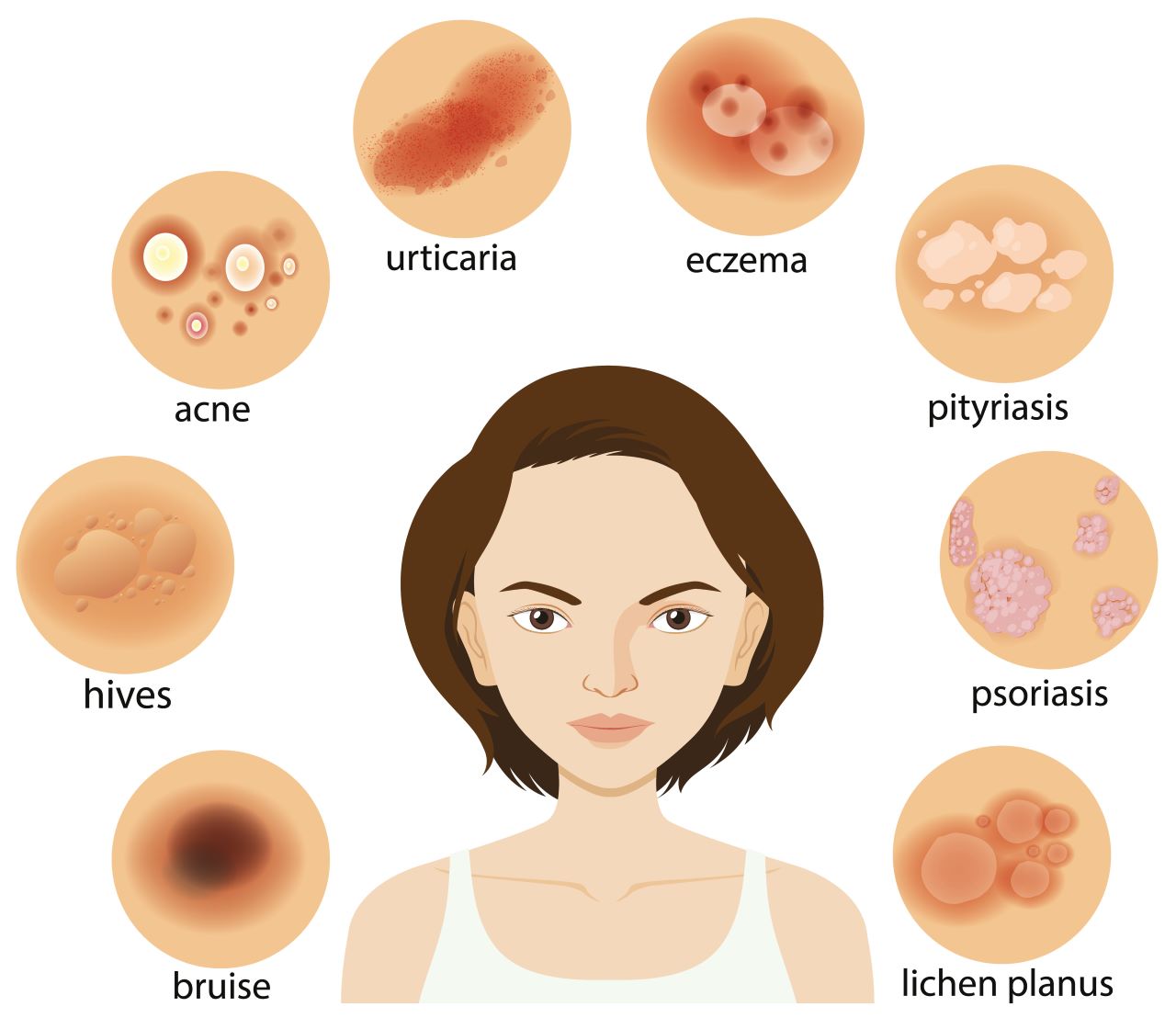
What is Eczema? Eczema is a non-contagious condition that causes the skin to become red, itchy, and inflamed. It’s often linked to a combination of genetic factors (a tendency toward sensitive skin and allergies) and environmental triggers. People with eczema often have a compromised skin barrier, meaning their skin loses moisture easily and is less effective at keeping out irritants and allergens.
Common Symptoms of Eczema:
- Intense Itching (Pruritus): This is the hallmark symptom and can be severe, especially at night, leading to sleep disruption.
- Dry Skin: Skin often feels rough, scaly, and very dry.
- Red to Brownish-Gray Patches: These can appear anywhere but are common on the hands, feet, ankles, wrists, neck, upper chest, eyelids, inside the bend of the elbows and knees. In infants, it often appears on the face and scalp.
- Small, Raised Bumps: These may leak fluid and crust over when scratched.
- Thickened, Cracked, Scaly Skin: With chronic scratching, the skin can become thickened (lichenification) and may crack, leading to pain and potential infection.
- Sensitive, Swollen Skin: Affected areas can be tender and swollen.
Eczema often follows a “flare-and-remit” cycle, meaning symptoms can worsen during flare-ups and then subside.
Triggers and Management Strategies in a Warm Climate
Common Triggers in Fort Myers and Beyond: While triggers vary, here are some common culprits, especially relevant in warm, humid environments:
- Irritants: Soaps, detergents, shampoos, disinfectants, prolonged contact with water (e.g., frequent swimming in chlorinated pools), and even certain fabrics like wool.
- Allergens: Dust mites, pollen (which is abundant in Fort Myers), pet dander, mold, and certain foods.
- Environmental Factors: Hot and humid weather (leading to sweat, which can be an irritant), sudden temperature changes, dry air (especially with air conditioning), and pollution.
- Stress: Emotional stress can trigger or worsen eczema flares.
- Sweat: In our climate, sweat can be a significant irritant for sensitive eczema-prone skin.
Management and Treatment Strategies:
- Moisturize, Moisturize, Moisturize: This is foundational. Apply thick, emollient creams or ointments (not lotions) at least twice daily, especially right after bathing to lock in moisture. Look for products labeled “fragrance-free” and “hypoallergenic.”
- Gentle Skin Care:
- Lukewarm Baths/Showers: Use lukewarm water, not hot, and limit bath time to 5-10 minutes.
- Mild Cleansers: Use gentle, fragrance-free cleansers instead of harsh soaps.
- Pat Dry: Gently pat skin dry with a soft towel, rather than rubbing.
- Identify and Avoid Triggers: Keep a “flare diary” to track potential triggers. For sweat-related issues, rinsing off after sweating and wearing breathable, loose-fitting cotton clothing can help.
- Manage Itching:
- Cold Compresses: Apply cool, wet compresses to itchy areas.
- Antihistamines: Oral antihistamines (e.g., diphenhydramine at night for sedation, or non-drowsy cetirizine/loratadine during the day) can help with itching.
- Keep Fingernails Short: To minimize skin damage from scratching.
- Topical Medications:
- Corticosteroid Creams/Ointments: These are common first-line treatments for inflammation and itching during flare-ups, available in various strengths. Use as directed by a healthcare professional.
- Calcineurin Inhibitors (e.g., tacrolimus, pimecrolimus): Non-steroidal options for sensitive areas or long-term maintenance.
- Advanced Treatments (for Severe Eczema):
- Phototherapy: Controlled exposure to UV light.
- Systemic Medications: Oral steroids, immunosuppressants, or newer biologic drugs (like dupilumab) for severe, widespread, or unresponsive eczema, often prescribed by a dermatologist.
A 2024 review in Dermatology Times emphasized the personalized nature of eczema treatment, highlighting the importance of working with a dermatologist to create an effective long-term management plan.
Conclusions and Key Takeaways
- Eczema is a chronic, non-contagious skin condition causing itchy, inflamed, and dry skin, often exacerbated by environmental factors like humidity and sweat in climates like Fort Myers.
- Symptoms include intense itching, red patches, dryness, and sometimes oozing blisters.
- Core management strategies include consistent moisturizing, gentle skin care, and identifying/avoiding personal triggers.
- OTC and prescription topical medications are key for managing flares, while advanced treatments exist for severe cases.
- Consult a dermatologist for persistent, severe, or complicated eczema.
Trusted References
Journal of the American Academy of Dermatology. (Refer to recent guidelines on eczema management.)
American Academy of Dermatology Association (AAD). www.aad.org (Refer to “Eczema” section.)
National Eczema Association (NEA). nationaleczema.org
Mayo Clinic. www.mayoclinic.org (Search for “Atopic Dermatitis” or “Eczema.”)

Recent Post
- The Liquid Advantage: Hydration, Thermogenesis, and Appetite Control
- The Hormonal Clock: Why Sleep is the Secret Ingredient to Fat Loss
- The Metabolic Shield: Preserving Muscle to Prevent Weight-Loss Rebound
- The Flamingo Test: Why You Should Stand on One Leg
- The “Natural Ozempic”: Why Fiber is the Hunger Crusher
This article reviewed by Dr. Jim Liu, MD.
There’s nothing more important than our good health – that’s our principal capital asset.
#medical #telehealth #umedoc #eczema #rash