Banishing the Itch: A Guide to Over-the-Counter Solutions for Common Fungal Skin Infections

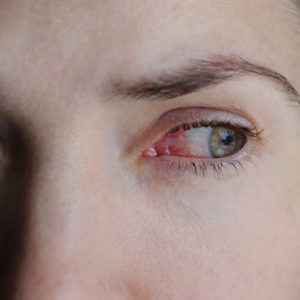
That relentless itch, the tell-tale scaling, or a spreading red ring on your skin – these are all classic signs of a fungal skin infection. From the gym to your own shower, these microscopic invaders can easily find a home on your body, leading to conditions like athlete’s foot, jock itch, and ringworm. While persistent, the good news is that most common fungal skin infections can be effectively tackled with accessible and potent over-the-counter (OTC) medications, available right here in Fort Myers.
This guide (updated for 2025) will help you understand the most common fungal culprits, choose the best OTC treatments, and implement effective self-care strategies for a swift return to comfortable, healthy skin.
Understanding the Common Fungal Invaders
What Are We Fighting? Fungal skin infections are caused by dermatophytes (fungi that feed on keratin in skin, hair, and nails) or yeasts (like Candida). They thrive in warm, moist, dark environments, making areas like feet, groin, and skin folds prime targets.
- Athlete’s Foot (Tinea Pedis): Characterized by itching, burning, scaling, redness, and sometimes blisters between toes or on the soles. Often contracted from locker rooms, pools, or shared footwear.
- Jock Itch (Tinea Cruris): A red, itchy, sometimes ring-shaped rash in the groin area, inner thighs, and buttocks. Common in athletes or those who sweat heavily.
- Ringworm (Tinea Corporis): A misnomer, as no worm is involved. It presents as a circular, red, itchy, scaly rash with raised borders and often clearer skin in the center. Can appear anywhere on the body.
- Cutaneous Candidiasis (Yeast Infection): Caused by Candida yeast, this typically appears in warm, moist skin folds (under breasts, armpits, abdomen) as a bright red rash with small, satellite lesions.
Risk Factors: High humidity (common in Fort Myers!), sweating, tight clothing, impaired immune system, diabetes, and communal showering.
Your Arsenal: Best OTC Antifungal Medications
OTC antifungals primarily work by either killing fungi (fungicidal) or preventing their growth (fungistatic). They are available in various forms (creams, sprays, powders, gels) to suit different needs and areas.
- Azole Antifungals (e.g., Clotrimazole, Miconazole, Ketoconazole):
- Common Brands: Lotrimin AF (Clotrimazole), Desenex (Miconazole), Nizoral A-D (Ketoconazole).
- Mechanism: These broad-spectrum antifungals disrupt the fungal cell membrane, stopping growth and ultimately killing the fungus.
- Best For: Effective against most common fungal skin infections including athlete’s foot, jock itch, ringworm, and often effective for yeast infections (check product specific indications).
- Allylamine Antifungals (e.g., Terbinafine, Naftifine):
- Common Brands: Lamisil AT (Terbinafine).
- Mechanism: Highly potent fungicidal agents that interfere with a key enzyme in the fungal cell wall synthesis pathway, directly killing the fungus.
- Best For: Considered particularly effective for dermatophyte infections (athlete’s foot, jock itch, ringworm) due to their fungus-killing action, often leading to shorter treatment courses (e.g., 1-2 weeks for athlete’s foot).
- Tolnaftate:
- Common Brands: Tinactin.
- Mechanism: Primarily works by inhibiting fungal growth.
- Best For: Athlete’s foot and ringworm. Often found in powders and sprays for preventative use or for milder cases.

Applying Your Treatment for Success:
- Clean and Dry First: Before each application, wash the affected area gently with soap and water, then dry thoroughly. This is crucial for effectiveness.
- Apply Thinly: Use a thin layer of cream or spray, extending slightly beyond the visible rash.
- Consistency is Key: Use the medication for the full recommended duration (e.g., 2-4 weeks), even if symptoms improve quickly. Stopping early is the primary cause of recurrence.
- Hygiene: Wash towels, bedding, and affected clothing in hot water. Avoid sharing personal items.
Preventing Recurrence and When to Seek Professional Help
Proactive Prevention Strategies:
- Keep Skin Dry: Especially in skin folds and between toes. Use absorbent powders if needed.
- Wear Breathable Materials: Cotton socks and underwear, loose-fitting clothing.
- Change Socks Regularly: Especially if you sweat.
- Footwear: Alternate shoes to allow them to dry out. Wear sandals or flip-flops in public showers, locker rooms, and around pools.
- Daily Hygiene: Shower after exercise and dry off completely.
When to Consult a Doctor: While OTCs are effective, seek medical advice if:
- The rash doesn’t improve significantly after 2-4 weeks of consistent OTC treatment.
- The infection is widespread or severe.
- The rash is on your scalp or nails (these almost always require prescription oral antifungals).
- You have a weakened immune system (e.g., diabetes, HIV).
- The rash is painful, oozing pus, or shows signs of bacterial infection (e.g., increased redness, warmth, fever).
- You are unsure of the diagnosis.
A 2025 consensus report from the American Podiatric Medical Association (APMA) emphasizes that early and accurate diagnosis is critical for effective management of fungal foot infections.
Conclusions and Key Takeaways
- Fungal skin infections are common and thrive in warm, moist conditions.
- Effective OTC medications include azoles (clotrimazole, miconazole) and allylamines (terbinafine), working to inhibit or kill fungi.
- Consistent application for the full recommended duration, along with keeping the area clean and dry, is paramount for successful treatment.
- Good hygiene and moisture control are essential for prevention.
- Consult a doctor if OTC treatment fails, the infection is severe, or involves the scalp/nails.
Trusted References
American Podiatric Medical Association (APMA). www.apma.org (For foot-related fungal infections.)
American Academy of Dermatology (AAD). www.aad.org (Refer to “Athlete’s Foot,” “Jock Itch,” “Ringworm” sections.)
Mayo Clinic. www.mayoclinic.org (Search for specific fungal infections.)
Centers for Disease Control and Prevention (CDC). www.cdc.gov/fungal/index.html

Recent Post
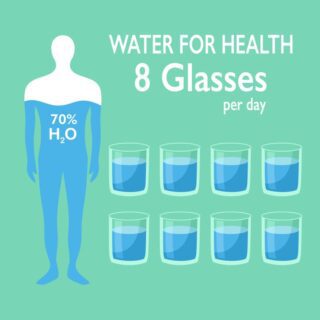
- The Liquid Advantage: Hydration, Thermogenesis, and Appetite Control
- The Hormonal Clock: Why Sleep is the Secret Ingredient to Fat Loss
- The Metabolic Shield: Preserving Muscle to Prevent Weight-Loss Rebound
- The Flamingo Test: Why You Should Stand on One Leg
- The “Natural Ozempic”: Why Fiber is the Hunger Crusher
This article reviewed by Dr. Jim Liu, MD.
There’s nothing more important than our good health – that’s our principal capital asset.
#medical #telehealth #umedoc # GLP #side effects